
DSME/T: The Gold Standard in Diabetes Education
Managing diabetes is a lot like caring for a newborn—relentlessly needy, impatient, and often irrational. It requires numerous daily decisions and a general high level of engagement and attention. I remember hearing at a professional conference that “if patients did everything their doctors asked of them it would take over 2.5 hours per day.” That’s a lot of time to be doing anything, let alone managing diabetes.
To best equip patients with tools to manage diabetes, the American Diabetes Association (ADA), American Association of Diabetes Care and Education Specialist (ADCES), and the Academy for Nutrition and Dietetics (AND) have updated their joint position statement on diabetes care and education.
The DSME/T Model
The joint position statement recommends the DSME/T model. Diabetes Self-Management Education and Training is a nationally-recognized set of standards when providing diabetes care and education. DSME/T objectives include: informed decision making, development of self-care behaviors, proficient problem solving, and active patient-provider collaboration.
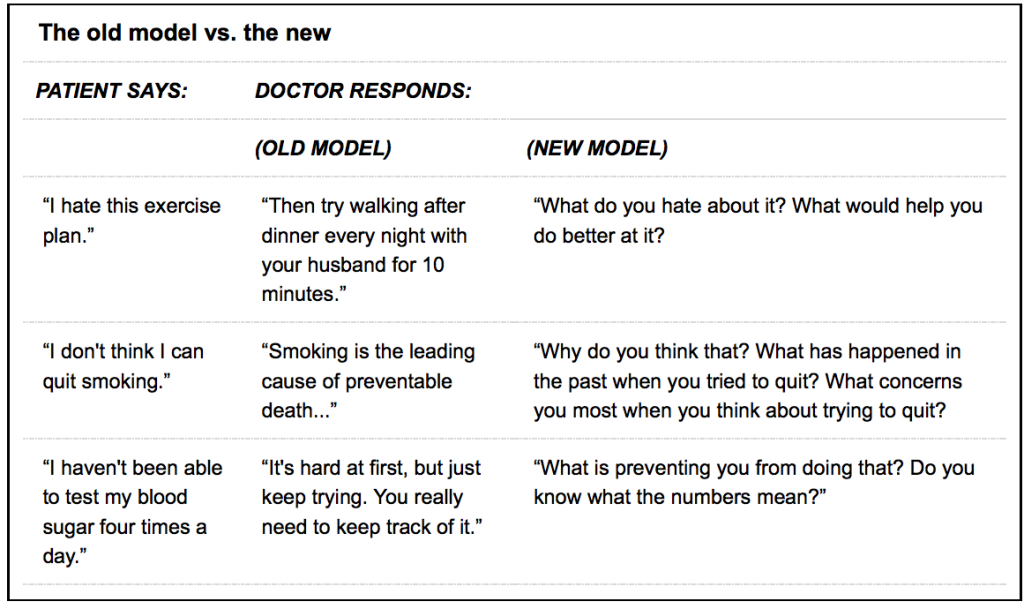
The approach is patient-centered. The focus is solution-based for day-to-day problems rather than disease etiology. It requires asking permission before advising and garnering a greater sense of what motivates patients to change.
Indicators of success are geared more towards behaviors—healthy eating, daily exercise, etc—than clinic outcomes like A1c or weight. Patients are in the driver’s seat of their own care.
Critical Points for DSME/T Referral
Expert suggest that there are four critical times to refer a patient for DSME/T services.
- At the onset of a new diabetes diagnosis
- Annually for health maintenance and prevention of complications
- At the onset of new complicating factors that influence self-management
- With a transition of care (ie. relocation, pediatric to adult care, etc.)
Of course, other situations may require additional attention to self-management needs. When in doubt—refer them out (to a diabetes educator, that is!).
Insurance Coverage
Albeit limited in hours, DSME/T is covered by Medicare, most state-run Medicaids, and a large number of commercial insurances. It’s incredibility cost-effective in reducing hospital admissions and re-admissions.
Coverage includes up to 10 hours the first year of diagnosis plus 2 hours each subsequent year for ongoing training. If rendered by a registered dietitian nutritionist, Medicare will cover 2-3 additional hours of diabetes-specific medical nutrition therapy (MNT). Medicaid and commercial insurance of MNT will vary.
Note, that both DSME/T and MNT must be provided by a clinician enrolled in an accredited diabetes education program. Programs can be accredited through either the American Diabetes Association (ADA) or the Association of Diabetes Care and Education Specialists (ADCES). Find a Diabetes Education Program in Your Area.
Barriers to DSME/T
Despite the overwhelming benefits of DSME/T, the Centers for Medicare Services (CMN) report that less than 7% of newly diagnosed individuals are referred for education. Even worse, less than 4% complete the 10 hours of covered training. Barries to participation are complex, but include:
- Patient/provider misunderstanding regarding the effectiveness of DSME/T
- Provider confusion on when and how to refer
- Lack of access to DSME/T services in the geographical area
- Patient psycho-social and behavioral factors
- Confusion regarding coverage and co-pays
While the list goes on, many of these barriers could be eliminated with better communication and promotion of DSME/T programs.
Adapting the DSME/T Model
DSME/T is a patient-centered approach to care. It empowers individuals to actively engage in their own treatment. Despite the barriers to utilization, it’s still one of the more effective tools in creating sustainable behavior change.

You May Also Like

CDCES and Primary Care: A Healthy Partnership
June 21, 2022
Product Review: Freestyle Libre 3
December 19, 2022
