Week 9: The Comprehensive NCP
I’ve finished my first week in clinical! My focus this week was to acclimate to the clinical setting, brush-up on disease states, and practice the NCP (Nutrition Care Process).
The Nutrtion Care Process is a systematic approach to providing nutrition care that improves consistency and predictability of outcomes. Similar to a Physician’s SOAP note, dietitians document the nutrition care process in an ADIME.
Step 1: Assessment
In the assessment, the dietitian examines components grouped into five categories; (1) nutrition-related history, (2) anthropometric measures, (3) labs, medical tests and procedures, (4) nutrition-focused physical findings and (5) client history.
Usually, the RD begins by talking with the patient or family to assess weight history, dietary patterns, allergies/intolerances, and nutrition concerns. The RD then reviews medical records, charts, and physician notes. I like to think of this as the “Sherlock Phase” where you have to think like a detective to gather as much information as possible.
Step 2: Nutrition Diagnosis
The second step in the NCP links the assessment with the intervention. The RD identifies and labels a specific nutrition diagnosis that the RD is then responsible for treating. This part can be tricky as patients rarely have “just one problem.” A simple problem left unaddressed can spiral into other problems. The challenge is determining where you think you can make the biggest improvement in nutritional health. Once determined, the diagnosis is written as PES statement (problem, etiology, symptoms).
Step 3: Nutrition Intervention
The third step includes planning and implementing a plan focused on the nutrition problem identified in the nutrition diagnosis. I would consider this the “fun” part for the dietitian. This step includes discussing with the resident and other members of the care team realistic goals and creating a plan to reach that goal. This could be providing nutrition education, behavior counseling, modified diets, or even tube feeds.
Step 4: Nutrition Monitoring and Evaluation
The final step is monitoring the progress that has been made by the resident. This final step links back to the first step as the RD assesses the progress made in weight status, meal intake, labs, and nutrition-focused physical findings. In areas like long-term care, an RD might monitor and evaluate for months. In the inpatient setting monitoring and evaluation ends at discharge. An initial, and 3-5 follow ups (depending on insurance coverage) seems to be the average in outpatient care.
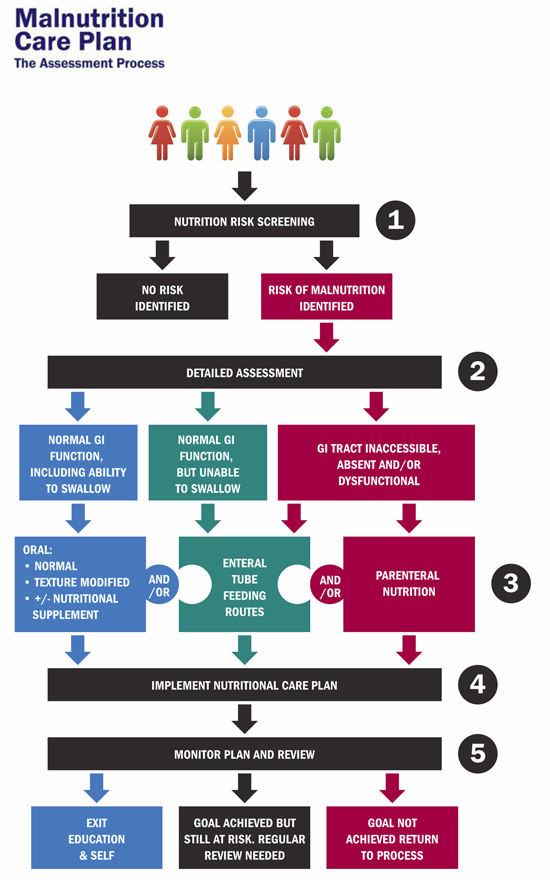
To put the Nutrition Care Process into context, I like this flow chart demonstrating how an RD might use an ADIME to address malnutrition.
Until next week,
S